- Biomarker-Driven Lung Cancer
- HER2 Breast Cancer
- Chronic Lymphocytic Leukemia
- Small Cell Lung Cancer
- Renal Cell Carcinoma

- CONFERENCES
- PUBLICATIONS
- CASE-BASED ROUNDTABLE

Case 1: 72-Year-Old Woman With Small Cell Lung Cancer

EP: 1 . Case 1: 72-Year-Old Woman With Small Cell Lung Cancer
Ep: 2 . case 1: extensive-stage small cell lung cancer background, ep: 3 . case 1: impower133 trial in small cell lung cancer, ep: 4 . case 1: caspian trial in extensive-stage small cell lung cancer, ep: 5 . case 1: biomarkers in small cell lung cancer, ep: 6 . case 1: small cell lung cancer in the era of immunotherapy.

EP: 7 . Case 2: 67-Year-Old Woman With EGFR+ Non–Small Cell Lung Cancer
Ep: 8 . case 2: biomarker testing for non–small cell lung cancer, ep: 9 . case 2: egfr-positive non–small cell lung cancer, ep: 10 . case 2: flaura study for egfr+ metastatic nsclc, ep: 11 . case 2: egfr+ nsclc combination therapies.

EP: 12 . Case 2: Treatment After Progression of EGFR+ NSCLC

EP: 13 . Case 3: 63-Year-Old Man With Unresectable Stage IIIA NSCLC
Ep: 14 . case 3: molecular testing in stage iii nsclc, ep: 15 . case 3: chemoradiation for stage iii nsclc, ep: 16 . case 3: pacific trial in unresectable stage iii nsclc, ep: 17 . case 3: standard of care in unresectable stage iii nsclc, ep: 18 . case 3: management of immune-related toxicities in stage iii nsclc.
Mark Socinski, MD: Thank you for joining us for this Targeted Oncology ™ Virtual Tumor Board ® focused on advanced lung cancer. In today’s presentations my colleagues and I will review three clinical cases. We will discuss an individualized approach to treatment for each patient, and we’ll review key clinical trial data that impact our decisions. I’m Dr. Mark Socinski from the AdventHealth cancer institute in Orlando, Florida. Today I’m joined by Dr Ed Kim, a medical oncologist from the Levine Cancer Institute in Charlotte, North Carolina; Dr Brendon Stiles, who is a thoracic surgeon from the Weill Cornell Medical Center in New York ; and Dr Tim Kruser, radiation oncologist from Northwestern Medicine Feinberg School of Medicine in Chicago. Thank you all for joining me today. We’re going to move to the first case, which is a case of small cell lung cancer. I’m going to ask Dr Kim to do the presentation.
Edward Kim, MD: Thanks, Mark. It’s my pleasure to walk us through the first case, which is small cell lung cancer. This is a case with a 72-year-old woman who presents with shortness of breath, a productive cough, chest pain, some fatigue, anorexia, a recent 18-pound weight loss, and a history of hypertension. She is a schoolteacher and has a 45-pack-a-year smoking history; she is currently a smoker. She is married, has 2 kids, and has a grandchild on the way. On physical exam she had some dullness to percussion with some decreased-breath sounds, and the chest x-ray shows a left hilar mass and a 5.4-cm left upper-lobe mass. CT scan reveals a hilar mass with a bilateral mediastinal extension. Negative for distant metastatic disease. PET scan shows activity in the left upper-lobe mass with supraclavicular nodal areas and liver lesions, and there are no metastases in the brain on MRI. The interventional radiographic test biopsy for liver reveals small cell, and her PS is 1. Right now we do have a patient who has extensive-stage small cell lung cancer. Unfortunately, it’s what we found. It’s very common to see this with liver metastases.
Transcript edited for clarity.

FDA Approval Marks Amivantamab's Milestone in EGFR+ NSCLC
In this episode, Joshua K. Sabari, MD, discusses the FDA approval of amivantamab plus chemotherapy as a first-line treatment for patients with EGFR exon 20 insertion mutation-positive non-small cell lung cancer.

Eftilagimod Alpha Combo Shows Promise in First-Line NSCLC
The phase 1 INSIGHT-003 trial showed that adding eftilagimod alpha to pembrolizumab and chemotherapy achieved a median overall survival of 32.9 months in metastatic non–small cell lung cancer.

Lisberg Discusses Dato-DXd's Role in Advanced Lung Cancer Care
In this episode of Targeted Talks, Aaron Lisberg, MD, discusses results from the phase 3 TROPION-Lung01 study of datopotamab in advanced or metastatic non–small cell lung cancer.

FDA Approval Sought for Dato-DXd in EGFR-Mutated NSCLC
A new BLA for datopotamab deruxtecan aims for FDA accelerated approval to treat EGFR-mutated NSCLC based on data from multiple TROPION trials, following FDA feedback.

NKTR-255 Shows Promise for Reversing Radiation-Induced Lymphopenia in NSCLC
NKTR-255 in combination with durvalumab following chemoradiation was well-tolerated in patients with non–small cell lung cancer, with a safety profile similar to earlier studies.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Lung Cancer: A Case Study
Submitted by Anna Stewart RN, BSN, MSN-C
Tags: cancer chemotherapy death end of life therapy treatment

Share Article:
Lung cancer is the number one cause of cancer-related death in men and the second most common in women. Lung cancer is responsible for 1.3 million deaths worldwide annually. The main types of lung cancers consist primarily of small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). In 2008, the National Cancer Institute (NCI) estimated in the United States that there were 215,020 new cases and 161, 840 cancer related deaths of SCLC and NSCLC combined. The most common cause of lung cancer is smoking. Other risk factors include genetics, radon gas, asbestos and air pollution which includes secondhand smoke.
Diagnostics is an important part of cancer treatment. Distinction between lung cancers is important because of the difference in treatments. Chest radiograph and computed tomography (CT scan) are used to visualize the lung cancer. A biopsy is done to confirm the diagnosis and usually achieved via bronchoscopy or CT guided biopsy. Categorization is done by viewing the cells under a microscope. NSCLC arises from epithelial cells and SCLC begins in the nerve cells or hormone-producing cells of the lung. The term “small cell” refers to the size and shape of the cancer cells as seen under a microscope. The histological classification of lung cancers is significant because it determines the type of treatment and prognosis, the stage (degree of metastasis), and patients performance status.
The frequency of NSCLC is 80.4% compared to 16.8% of cases of SCLC. Other types of lung cancers (carcinoid, sarcoma and unspecified lung cancers) are less than 3%. Surgery, chemotherapy, and radiotherapy are possible treatments. The NCI states that the five year survival rate is 15% with treatment.
SCLC has the poorest prognosis of lung cancer because it is the fastest growing and has usually metastasized by the time a diagnosis is made. Although lung cancer can metastasize anywhere in the body, the most common sites are the lymph nodes, lungs, bones, brain, liver, and the adrenal glands. Metastases from lung cancer can cause additional difficulties such as breathing problems, bone pain, abdominal or back pain, headache, weakness, seizures, and/or speech difficulties. Lung tumors can release hormones that result in chemical imbalances, such as low blood sodium levels or high blood calcium levels, but this is uncommon (NCI, 2008).
Staging of small cell lung cancer
Because almost all small cell lung cancer has spread outside the lung when discovered, very few patients with small cell lung cancer are treated with surgery, and all receive chemotherapy. Some patients with small cell lung cancer can benefit from radiation therapy. The staging for small cell lung cancer helps identify which patients can be treated with radiation therapy in addition to chemotherapy. Small cell lung cancer is classified as either limited stage or extensive stage:
- Limited stage means the cancer is located on one side of the chest and involves a single region of the lung and adjacent lymph nodes. This region can be treated in its entirety with radiation therapy. About 30% of patients have limited stage.
- Extensive stage means the cancer has spread to other regions of the chest, or outside of the chest, and cannot be treated completely with radiation therapy. Most patients (70%) have extensive stage disease and are treated with chemotherapy only (McCance, 2006).
Treatment of small cell lung cancer
The treatment of small cell lung cancer depends on the stage. Small cell lung cancer spreads quickly, so systemic chemotherapy is the primary treatment for all patients. The most commonly used chemotherapy regimen is etoposide (VePesid, Lastet, Etopoph plus cisplatin (Platinol) or carboplatin (Paraplatin). Patients with limited stage small cell lung cancer are best treated with simultaneous chemotherapy plus radiation therapy to the chest given twice a day. Radiation therapy is best when given during the first or second month of chemotherapy. Patients with extensive stage cancer are treated with chemotherapy only. Chemotherapy is given for three to six months. Surgery is rarely appropriate for patients with small cell lung cancer and is only considered for patients with very early-stage disease, such as a small lung nodule. In those cases, chemotherapy, with or without radiation therapy is given afterwards.
In patients whose tumors have diminished after chemotherapy, radiation therapy to the head cuts the risk that the cancer will spread to the brain. This preventative radiation to the head is called prophylactic cranial irradiation (PCI) and has been shown to extend the lives of these patients.
Like patients with advanced NSCLC, patients with small cell lung cancer of any stage face the risk that the cancer can return, even when it is initially controlled. All patients with small cell lung cancer must be followed closely by their doctors with x-rays, scans, and check-ups.
Most patients with lung cancer are treated by more than one specialist with more than one type of treatment. For example, chemotherapy can be prescribed before or after surgery, or before, during, or after radiation therapy. Patients should have a sense that their doctors have a coordinated plan of care and are communicating effectively with one another. If patients do not feel that the surgeon, radiation oncologist, or medical oncologist is communicating effectively with them or each other about the goals of treatment and the plan of care, patients should discuss their concerns with their doctors or seek additional opinions before treatment (Roman & Brigham, 2007).
Radiation therapy
Radiation therapy is the use of high energy x-rays or other particles to kill cancer cells. Radiation therapy is performed by a specialist called a radiation oncologist. Like surgery, radiation therapy cannot be used to treat widespread cancer. Radiation only kills cancer cells directly in the path of the radiation beam. It also damages the normal cells caught in its path, and for this reason, it cannot be used to treat large areas of the body. Patients with lung cancer treated with radiation therapy often experience fatigue and loss of appetite. If radiation therapy is given to the neck, or center of the chest, patients may also develop a sore throat and have difficulty swallowing. Skin irritation, like sunburn, may occur at the treatment site. Most side effects go away soon after treatment is finished.
If the radiation therapy irritates or inflames the lung, patients may develop a cough, fever, or shortness of breath which may begin months or years after the radiation therapy. This condition occurs in about 15% of patients and is called radiation pneumonitis. If it is mild, radiation pneumonitis does not require treatment and resolves on its own. If it is severe, radiation pneumonitis may require treatment with steroid medications, such as prednisone. Radiation therapy may also cause permanent scarring of the lung tissue near the site of the original tumor. Typically, the scarring does not lead to symptoms. Widespread scarring can lead to permanent cough and shortness of breath. For this reason, radiation oncologists carefully plan the treatments using CT scans of the chest to minimize the amount of normal lung tissue exposed to the radiation beam (Wikipedia, 2009).
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells. Systemic chemotherapy is delivered through the bloodstream, targeting cancer cells throughout the body. Chemotherapy is given by a medical oncologist. Most chemotherapy used for lung cancer is given intravenously. The side effects of chemotherapy depend on the individual and the dose used, but can include fatigue, risk of infection, nausea and vomiting, loss of appetite, and diarrhea. Nausea and vomiting are often avoidable; for more information, read the What to Know: ASCO's Guideline on Preventing Nausea and Vomiting Caused by Cancer Treatment. These side effects usually go away once treatment is finished.
Chemotherapy may also damage normal cells in the body, including blood cells, skin cells, and nerve cells. This may result in low blood counts, an increased risk of infection, hair loss, mouth sores, and/or numbness or tingling in the hands and feet. Your medical oncologist can often prescribe drugs to help provide relief from many side effects. Hormone injections are also used to prevent white and red blood cell counts from becoming too low.
Newer chemotherapies cause fewer side effects and are as effective as older treatments. Chemotherapy has been shown to improve both the length and quality of life in people with lung cancer of all stages.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions through Cancer.Net's Drug Information Resources, which provides links to searchable drug databases (Swierzewski, 2007).
DH is a 70 year old female with a diagnosis of small cell carcinoma of the lung limited stage disease. The patient was diagnosed August, 2007 and treated from 10/2007 through 11/2007 with Carboplatin and VP16. The patient had no response to the initial treatment. She was subsequently treated Carboplatin and Taxol from 12/2007 through 3/2008.
After completion of chemotherapy plans were made for her to receive radiation therapy. The plans for radiation were delayed due to the discovery of a parotid tumor. This tumor was identified as a Warthin’s tumor (benign neoplasm of the salivary glands). The patient did receive radiation therapy from 7/2008 to 10/2008. Dosing of 5,580 cGy (cGy= centigray, the gray measures the deposited energy of radiation) and 31 fractions (the smaller, divided doses of radiation that are given each day) was administered over 70 days.
DH has been off chemotherapy since 3/2008 and radiation therapy since 10/2008 with no further treatment. DH returns today in follow up. She has had a relatively stable weight and good appetite. The patient had a mammogram, CT/Abd-Pelvis and chest x-ray on February 3, 2009. All were normal with the exception of a slight prominence of the left hilum thought to be related to original tumor. Patient also had colonoscopy and endoscopy done on 3/30/2009. The endoscopy was negative but the colonoscopy was positive for diverticuli. PET CT done on 3/25/2009 at local hospital showed areas of enlarged nodes located around the bronchial tree, abdomen and left axillary. DH is to return to her primary care physician (PCP) to have an area in the abdomen removed and biopsied. She has an appointment with the PCP on Friday, April 10, 2009. She does complain of non-exertional chest pain and has a history of hypertension. DH does have some general medical arthritis as well as paresthesias and numbness from Taxol therapy.
Patient’s labs values are stable with Hgb of 12.6, and Hct 39.1. Platelets have improved from previous visit from 312 to 371. White blood cell count continues to improve as well up from 7.52 to 8.0. Lymphocytes and monocytes are stable at 14 and 9 prospectively.
Explanations are given to DH and her husband regarding the possibility of further chemo and radiation therapies pending biopsy results. Patient and husband verbalize understanding and agree to plan of care. Biopsy is scheduled with PCP in two days. Patient scheduled for follow up visit with oncologist in two weeks.
- Brashers, V. (2006). Alterations of Pulmonary Function (pp.1237-1243). In McCance, Pathophysiology The Biologic Basis for Disease in Adults and Children (5th ed.)St. Louis, Mosby Elsevier.
- National Cancer Institute (2009). Small Cell Lung Cancer Treatment (PDQ),
- Retrieved April 13, 2009 from: meb.uni-bonn.de/cancer.gov.
- Roman, J., & Brigham, K., (2007) Neoplastic Disorders of the Lung (pp259-263),
- Andreoli and Carpenter’s: Cecil Essentials of Medicine (7th ed.), Philadelphia, W.B. Sanders Company.
- Swierzewski, S. (2007). Chemotherapy. Retrieved April 13, 2009 from: oncologychannel.com.
- Wikipedia (2009). Lung Cancer, Retrieved April 22, 2009 from: wikipedia.org.
Career Opportunities

More Like This

An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Effects of high quality nursing in patients with lung cancer undergoing chemotherapy and related influence on self-care ability and pulmonary function
- Author information
- Article notes
- Copyright and License information
Address correspondence to: Han Wang, Department of Oncology Chemotherapy Day Ward, Peking Union Medical College Hospital, No. 1 Shuaifuyuan, Dongdan North Street, Dongcheng District, Beijing 100010, China. Tel: +86-010-69151287; Fax: +86-010-69151287; E-mail: [email protected]
Received 2021 Jan 29; Accepted 2021 Feb 24; Collection date 2021.
Objective: To explore the effects of high quality nursing in patients with lung cancer undergoing chemotherapy and related influence on self-care ability and pulmonary function. Methods: 108 patients with lung cancer were grouped as the control group (54 cases, received routine nursing) and the observation group (54 cases, received high quality nursing including health education, psychological nursing, diet intervention, pain nursing and complication nursing). The psychology, self-care ability, pulmonary function, quality of life and complications before and after the intervention were compared. Results: After 2 months of intervention, peak expiratory flow (PEF), percentage of forced vital capacity (FVC%) and the ratio of forced expiratory volume in 1 second to forced vital capacity (FEV 1 /FVC) of the two groups were all largely increased, and the observation group had even higher indexes than the control group (all P<0.05). Compared with before intervention, Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD) scores of the two groups both decreased after 2 months of intervention, and the observation group had lower score than the control group. The score of Exercise of Self-care Agency (ESCA) Scale and the quality of life questionnaire-C30 formulated by the European Organization for research and treatment of cancer (EORTC QLQ-C30) in the two groups were both elevated after the intervention and the observation group had higher scores than the control group (all P<0.05). The observation group had much lower total incidence of adverse reactions than the control group during chemotherapy (P<0.05). Conclusion: High quality nursing for patients with lung cancer undergoing chemotherapy effectively alleviates the bad mood and improves the quality of life and lung function, which is worthy of clinical application.
Keywords: High quality nursing, lung cancer, self-care ability, psychology, pulmonary function

Introduction
Lung cancer is a malignancy with relatively high morbidity. The World Health Organization (WHO) reported that lung cancer related death was as high as 1.1 million per year, accounting for 17.8% of all cancer related death. Up to now, the morbidity of lung cancer is increasing year by year [ 1 ]. One of the main treatments for lung cancer is chemotherapy, which needs a long process and is always accompanied with obvious side effects. In the process of chemotherapy, some patients have different degrees of psychological disorders, which not only affect the effect of chemotherapy, but also reduce the quality of life of patients [ 2 ]. Therefore, it is of great significance to provide scientific and high-quality nursing for patients during chemotherapy to improve their bad emotions and quality of life.
High quality nursing is patient-centered and it strengthens the basic nursing and nursing responsibility, thus providing the patients with “high quality and efficient” medical services. High quality nursing has been widely used in many clinical departments, and shows good therapeutic effect. Mendes et al. reported that high quality nursing improved the cardiac function of patients with coronary heart disease, and also helped to enhance the treatment compliance [ 3 ]. Burton et al. demonstrated that high quality nursing improved the postoperative quality of life of patients with gastric cancer resection [ 4 ]. However, research about the effects of high-quality nursing on self-care ability of lung cancer patients during chemotherapy is extremely rare. It is also unknown whether different nursing methods have different effects on lung function of lung cancer patients. Therefore, this study explored the effects of high-quality nursing in patients with lung cancer undergoing chemotherapy, and analyzed its impact on patients’ self-care ability and lung function.
Materials and methods
General materials.
108 cases of lung cancer patients admitted in our hospital from December 2018 to February 2020 were selected as the research objects. These patients were grouped into the control group and the observation group according to the random number table method. Inclusion criteria: Patients aged between 35-75 years; patients confirmed by pathological biopsy as lung cancer in accordance with the “Diagnosis and treatment of primary lung cancer (2011 Edition)”; patients received chemotherapy [ 5 ]; Karnofsky (KPS) scores ≥70; life expectancy > 3 month; patients signed the informed consent. Exclusion criteria: Patients with other malignant tumors; patients with chemotherapy contraindications or allergic to the drugs used in this study; patients complicated with cerebral embolism, cerebral hemorrhage and other serious medical diseases; patients with abnormal liver and kidney function or obvious organic lesions; patients with diseases of immune system, blood system and endocrine system; patients participated in other researchers, etc. This study was approved by the medical ethics committee of our hospital.
Patients in both groups received chemotherapy and took gemcitabine (Nanjing Zhengda Tianqing Pharmaceutical Co., Ltd., specification: 1.0 g, origin: China) intravenously at the dose of 1,000-1,250 mg/m 2 on the 1st and 8th day; patients were also treated with Cisplatin (Jiangsu Haosen Pharmaceutical Group Co., Ltd., specification: 6 mL: 30 mg, origin: China) intravenously at the dose of 25 mg/m 2 from day 1 to day 3; patients also took gefitinib tablets (Jiangsu Hengrui Pharmaceutical Co., Ltd., specification: 0.25 g, origin: China) orally, 0.25 g/day, once a day. In addition, palonosetron hydrochloride injection (Jiangsu aosaikang Pharmaceutical Co., Ltd., specification: 5 mL: 0.25 mg based on palonosetron, origin: China) was given intravenously every day to prevent vomiting. 21 days were taken as a course of chemotherapy and the patients needed 2 courses continuously.
Patients in the control group received routine nursing during chemotherapy: follow the doctor’s advice and cooperate with clinicians to implement chemotherapy; take oral analgesics to relieve pain; have more meals a day but less food at each time; take light and digestible diet and have more water; follow the discharge guidance, etc.
Patients in the observation group received high quality nursing: (1) Health education: nurses explain lung cancer related knowledge, treatment measures, possible adverse reactions and countermeasures to patients; (2) Psychological nursing: cancer patients are prone to various degrees of bad psychology induced by many factors, such as tension and anxiety, which need the nurses to communicate with the patients more frequently [ 6 ]. Not the disease, but some daily interesting things are included in the chat. In the process of chatting, nurses could learn about the emotional fluctuation of patients. The nurses or counselors should give targeted psychological counseling according to the specific situation of patients, so as to eliminate the negative emotions of patients and encourage the patients to actively cooperate with the treatment; (3) Dietary intervention: patients with advanced cancer are often accompanied with malnutrition, so it is very important to give reasonable dietary intervention to maintain the nutrition needed by patients with advanced cancer and to improve their malnutrition [ 7 ]. Nutritionists can evaluate the nutritional status of patients according to the clinical examination results, and give targeted dietary advice according to the dietary guidance for patients with malignant tumor (Health industry standard of the People’s Republic of China No.: WS/T 559-2017) based on the specific situation of patients. The patients were instructed to take food containing more proteins and vitamins to ensure the protein intake of 1 kcal/(kg·d)-1.2 kcal/(kg·d). The energy supply of fat and carbohydrate should account for 35-50% of the total energy. Adults should eat 200-400 g of cereals every day, take more fruits and milk, try to adopt the low-fat diet and reduce cholesterol intake. In addition, alcohol and spicy food should be forbidden during chemotherapy; (4) Pain care: lung cancer patients are prone to bone metastasis, which causes pain. Thus, timely analgesic measures should be given to patients with obvious pain. Pethidine or morphine can be used for patients with moderate to severe pain and fentanyl transdermal patch or PCs could be used for patients with severe pain; (5) Complications nursing: chemotherapy is often accompanied by obvious gastrointestinal reactions such as nausea, vomiting and hematotoxic side effects such as bone marrow suppression [ 8 ]. Therefore, appropriate measures should be taken to prevent the occurrence of complications, such as tropisetron or palonosetron for antiemetic before chemotherapy, and colony-stimulating factor for the suppression of bone marrow suppression caused by chemotherapy. At the same time, the blood routine and liver and kidney function of patients should be checked regularly and the dosage of chemotherapy drugs should be adjusted in time in case of abnormality.
Outcome measures
Main outcome measures.
The observation time was set as before the intervention and 2 months after the intervention.
(1) Pulmonary function: the peak expiratory flow (PEF), percentage of forced vital capacity (FVC%) and the ratio of forced expiratory volume in 1 second to forced vital capacity (FEV 1 /FVC) were measured by the pulmonary function instrument (Guangzhou Aoxun Instrument Co., Ltd., China).
(2) Psychology: Psychology was evaluated by Hamilton Anxiety Scale and Hamilton Depression Scale (HAMA, HAMD) [ 9 , 10 ]. HAMA ≥7 indicates that the patient may have anxiety, and HAMA <7 indicates that the patient has no anxiety; HAMD (17 items) scores 7-17 suggests that the patient may have depression symptoms; HAMD <7 suggests that the patient has no depression symptoms. The degree of anxiety and depression increased with the score.
(3) Self-care ability: self-care ability was scored according the Exercise of Self-care Agency (ESCA) scale, with a total of 172 points. The higher the score is, the stronger the self-care ability of the patient is [ 11 ].
Secondary outcome measures
(1) The adverse reactions such as gastrointestinal reactions, myelosuppression, alopecia, hepatotoxicity, nephrotoxicity and neurotoxicity were compared between the two groups during chemotherapy. The total incidence of adverse reactions was calculated as the number of adverse reactions/total cases ×100%. (2) Quality of life: quality of life was evaluated by the quality of life questionnaire-C30 formulated by the European Organization for research and treatment of cancer (EORTC QLQ-C30) [ 12 ]. It contains four dimensions including functional domain, symptom domain, overall quality of life domain and single item, with 100 points per dimension. The higher the score is, the better the quality of life is.
Statistical analysis
SPSS 20.0 was used for data analysis. The enumeration data were expressed as n (%) and were compared by chi square test; measurement data were shown in x̅ ± sd. Paired t-test was used for comparison before and after intervention, and independent t-test was used for comparison between the two groups. P<0.05 means that the difference is statistically significant.
Comparison of general information between the two groups
No significant difference existed in the general information between the two groups (P > 0.05) and the two groups were comparable. See Table 1 for details.
General information of the two groups (n, x̅ ± sd)
Note: KPS: Karnofsky.
Pulmonary function
After 2 months of intervention, PEF, FVC% and FEV 1 /FVC of the two groups were all significantly increased, and the observation group had higher indexes than the control group (all P<0.05). See Table 2 for details.
Pulmonary function of the two groups before and after intervention (x̅ ± sd)
Note: PEF: peak expiratory flow; FVC%: percentage of forced vital capacity; FEV 1 /FVC: the ratio of forced expiratory volume in 1 second to forced vital capacity.
P<0.05 compared with before the intervention;
P<0.05 compared with the control group after the intervention.
Compared with before intervention, HAMA and HAMD scores of the two groups both decreased after 2 months of intervention, and the observation group had lower scores than the control group (both P<0.05). See Table 3 for details.
HAMA and HAMD scores of the two groups before and after the intervention (x̅ ± sd, score)
Note: HAMA: Hamilton Anxiety Scale; HAMD: Hamilton Depression Scale.
The scores of exercise of self-care agency (ESCA)
Compared with before intervention, the scores of self-concept, self-care skills, self-responsibility and health knowledge level of the two groups all increased after the intervention, and the observation group had higher scores than the control group (all P<0.05). See Table 4 for details.
ESCA scores of the two groups before and after the intervention (x̅ ± sd, score)
Note: ESCA: Exercise of Self-care Agency.
Adverse reaction
During chemotherapy, the total incidence of adverse reactions in the observation group was 9.26% (1 case of gastrointestinal reaction, 2 cases of myelosuppression and 2 cases of alopecia), which was significantly lower than 24.07% in the control group (3 cases of gastrointestinal reaction, 3 cases of myelosuppression, 4 cases of alopecia, 1 case of hepatotoxicity, 1 case of nephrotoxicity and 1 case of neurotoxicity) (P<0.05). See Figure 1 for details.
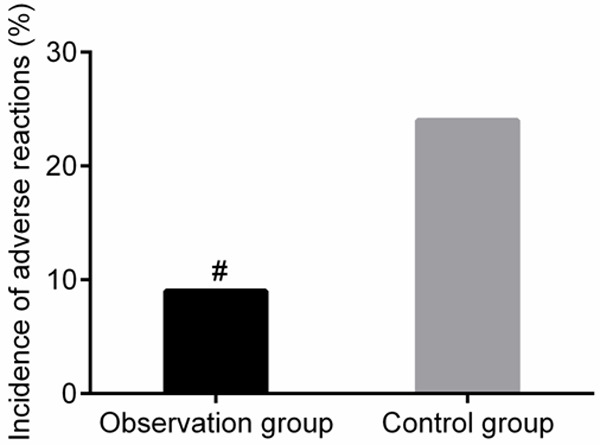
Adverse reaction of the two groups during chemotherapy. #P<0.05 compared with the control group.
Quality of life
Two months after the intervention, the EORTC QLQ-C30 scores in each dimension of the two groups were all higher than those before the intervention. At the same time, the observation group had higher scores than the control group (all P<0.05). See Table 5 for details.
EORTC QLQ-C30 scores of the two groups in each dimension before and after intervention (x̅ ± sd, score)
Note: EORTC QLQ-C30: the quality of life questionnaire-C30 formulated by the European Organization for research and treatment of cancer.
The morbidity of lung cancer is gradually increasing due to various factors such as environmental pollution and smoking. As one of the main treatment measures, chemotherapy is followed by various toxic and side effects which reduce the treatment compliance of some patients. Some patients even give up the treatment because of intolerable adverse reactions [ 13 ]. Therefore, high quality nursing during chemotherapy is very helpful for reducing chemotherapy related complications and improving prognosis. Stewart et al. showed that different nursing methods had different effects on lung function of lung cancer patients [ 14 ]. In this study, the improvement of lung function indexes in the observation group was better than that in the control group after 2 months of intervention, suggesting that high-quality nursing significantly improved lung function for lung cancer patients undergoing chemotherapy compared with the conventional nursing. Health education in the high quality nursing helps the patients understand the necessity and importance of actively cooperating with the treatment, which improves the treatment compliance of patients. Therefore, high quality nursing is conducive to improving the clinical effects of chemotherapy, and better improves the lung function of patients.
Self-care ability refers to the ability of patients to take care of themselves during illness. Previous study pointed out that the level of self-care ability of patients directly determined their self-efficacy, and the enhancement of self-efficacy of patients further promoted the prognosis [ 15 ]. In this study, the scores of self-concept, self-care skills, self-responsibility and health knowledge in the observation group were higher than those in the control group after the intervention, suggesting that the implementation of high-quality nursing can significantly improve the self-care ability of lung cancer patients receiving chemotherapy. Similar conclusions were also found in the study of Brown et al., which pointed out that high-quality nursing enhanced patients’ self-care ability and self-efficacy compared with conventional nursing measures [ 16 ]. The high-quality nursing in this study is more comprehensive and scientific in many aspects, such as health education, psychological nursing, diet intervention, pain nursing and complication nursing. At the same time, patients have a more comprehensive understanding of lung cancer related knowledge, treatment measures, possible adverse reactions and coping measures through health education, which is helpful to enhance the treatment compliance of patients and improve the self-care ability of patients [ 17 ].
Affected by many factors such as chemotherapy adverse reactions, cancer pain and the prognosis, most cancer patients may have different degrees of adverse psychological state, and even develop into depression. Some patients may even have suicidal thoughts, resulting in a significant decline in quality of life [ 18 ]. A study pointed out that up to 75% of patients with advanced cancer might have psychological disorder, which not only affects the effects of radiotherapy and chemotherapy, but also reduces the treatment compliance of patients [ 19 ]. In this study, patients in the observation group had lower HAMA and HAMD scores and higher EORTC QLQ-C30 scores of each dimension than those of the control group after 2 months of intervention, suggesting that high-quality nursing strongly improves the anxiety, depression and other adverse psychological states, and improves the quality of life for lung cancer patients receiving chemotherapy. Griffiths et al. also found that high-quality nursing improved the quality of life of cancer patients [ 20 ]. Adam et al. also found that the psychological state of cancer patients with obvious psychological disorders was significantly improved after receiving the high-quality nursing [ 21 ]. In addition to the routine nursing of pain and complications, high-quality nursing also pays attention to the psychological counseling of patients. The nurses can capture emotional fluctuations of patients in time through communication and conduct targeted psychological counseling, thus improving the bad psychological state and quality of life of patients [ 22 ]. In addition, our present study also found that the observation group had lower incidence of complications during chemotherapy than the control group, suggesting that high-quality nursing can largely reduce the incidence of complications for lung cancer patients receiving chemotherapy. However, this study is a single center study with limited sample size, thus further study is needed to confirm the effects of high-quality nursing on long-term lung function and self-care ability of patients.
In conclusion, high quality nursing effectively alleviates the bad mood, improves the quality of life and lung function, and reduces the risk of complications for lung cancer patients with chemotherapy, which is worthy of clinical application.
Disclosure of conflict of interest
- 1. Huang F, Pan B, Wu J, Chen E, Chen L. Relationship between exposure to PM2.5 and lung cancer incidence and mortality: a meta-analysis. Oncotarget. 2017;8:43322–43331. doi: 10.18632/oncotarget.17313. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Nagasaka M, Gadgeel SM. Role of chemotherapy and targeted therapy in early-stage non-small cell lung cancer. Expert Rev Anticancer Ther. 2018;18:63–70. doi: 10.1080/14737140.2018.1409624. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Mendes A. Coronary heart disease: self-care, communication and quality of life. Br J Community Nurs. 2015;20:42. doi: 10.12968/bjcn.2015.20.1.42. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Burton PR, Ooi GJ, Shaw K, Smith AI, Brown WA, Nottle PD. Assessing quality of care in oesophago-gastric cancer surgery in Australia. ANZ J Surg. 2018;88:290–295. doi: 10.1111/ans.13752. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Zhi XY, Liu DR, Chen DH, Yang Y, Du X, Bu H, Zhou QH, Jiang GN, Han BH, Cheng G. Chinese guidelines on the diagnosis and treatment of primary lung cancer (2011 Version) Chin J Lung Cancer. 2012;15:677–688. doi: 10.3779/j.issn.1009-3419.2012.12.01. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Greer S, Ramo D, Chang YJ, Fu M, Moskowitz J, Haritatos J. Use of the chatbot “vivibot” to deliver positive psychology skills and promote well-being among young people after cancer treatment: randomized controlled feasibility trial. JMIR Mhealth Uhealth. 2019;7:e15018. doi: 10.2196/15018. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Wiseman MJ. Nutrition and cancer: prevention and survival. Br J Nutr. 2019;122:481–487. doi: 10.1017/S0007114518002222. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Heinrich S, Lang H. Neoadjuvant therapy of pancreatic cancer: definitions and benefits. Int J Mol Sci. 2017;18:1622–1629. doi: 10.3390/ijms18081622. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Zimmerman M, Martin J, Clark H, McGonigal P, Harris L, Holst CG. Measuring anxiety in depressed patients: a comparison of the hamilton anxiety rating scale and the DSM-5 anxious distress specifier interview. J Psychiatr Res. 2017;93:59–63. doi: 10.1016/j.jpsychires.2017.05.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Raimo S, Trojano L, Spitaleri D, Petretta V, Grossi D, Santangelo G. Psychometric properties of the hamilton depression rating scale in multiple sclerosis. Qual Life Res. 2015;24:1973–1980. doi: 10.1007/s11136-015-0940-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Gao H, Söderhamn U, Cliffordson C, Guo L, Guo Q, Liu K. Reliability and validity of the Chinese version of the self-care ability scale for the elderly. J Clin Nurs. 2017;26:4489–4497. doi: 10.1111/jocn.13779. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Nolte S, Liegl G, Petersen MA, Aaronson NK, Costantini A, Fayers PM, Groenvold M, Holzner B, Johnson CD, Kemmler G, Tomaszewski KA, Waldmann A, Young TE, Rose M. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur J Cancer. 2019;107:153–163. doi: 10.1016/j.ejca.2018.11.024. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Rossi A, Di Maio M. Platinum-based chemotherapy in advanced non-small-cell lung cancer: optimal number of treatment cycles. Expert Rev Anticancer Ther. 2016;16:653–660. doi: 10.1586/14737140.2016.1170596. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Stewart I, Leary A, Tod A, Borthwick D, Khakwani A, Hubbard R, Beckett P, Tata LJ. Barriers to delivering advanced cancer nursing: a workload analysis of specialist nurse practice linked to the English national lung cancer audit. Eur J Oncol Nurs. 2018;36:103–111. doi: 10.1016/j.ejon.2018.07.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Raffaele B, Biagioli V, Cirillo L, De Marinis MG, Matarese M. Cross-validation of the selfcare ability scale for elderly (SASE) in a sample of Italian older adults. Scand J Caring Sci. 2018;32:1398–1408. doi: 10.1111/scs.12585. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Brown E, Milosevic M. Quality in cancer care: lessons from the Canadian partnership for quality radiotherapy. Healthc Manage Forum. 2018;31:18–21. doi: 10.1177/0840470417716684. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Reade CJ, Elit LM. Current quality of gynecologic cancer care in North America. Obstet Gynecol Clin North Am. 2019;46:1–17. doi: 10.1016/j.ogc.2018.09.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Ismail MF, Lavelle C, Cassidy EM. Steroid-induced mental disorders in cancer patients: a systematic review. Future Oncol. 2017;13:2719–2731. doi: 10.2217/fon-2017-0306. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Yang YL, Liu L, Li MY, Shi M, Wang L. Psychological disorders and psychosocial resources of patients with newly diagnosed bladder and kidney cancer: a cross-sectional study. PLoS One. 2016;11:e0155607. doi: 10.1371/journal.pone.0155607. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Griffiths RI, Keating NL, Bankhead CR. Quality of diabetes care in cancer: a systematic review. Int J Qual Health Care. 2019;31:75–88. doi: 10.1093/intqhc/mzy124. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Adam C, Patiraki E, Lemonidou C, Radwin L, Charalambous A, Charalambous M, Berg A, Sjövall K, Katajisto J, Stolt M, Suhonen R. Quality of nursing care as perceived by cancer patients: a cross-sectional survey in four European countries. J Buon. 2017;22:777–782. [ PubMed ] [ Google Scholar ]
- 22. Siembida EJ, Kadan-Lottick NS, Moss K, Bellizzi KM. Adolescent cancer patients’ perceived quality of cancer care: the roles of patient engagement and supporting independence. Patient Educ Couns. 2018;101:1683–1689. doi: 10.1016/j.pec.2018.04.002. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- PDF (274.7 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
Dr. Jonathan E. Eisen: A 47-year-old woman presented to this hospital early during the pandemic of coronavirus disease 2019 (Covid-19), the disease caused by severe acute respiratory syndrome...
The phase 3 SKYSCRAPER-01 trial of tiragolumab and atezolizumab in PD-L1-high non–small cell lung cancer did not meet its primary end point of overall survival.
Lung cancer is the number one cause of cancer-related death in men and the second most common in women. Lung cancer is responsible for 1.3 million deaths worldwide annually. Journal of Nursing
What nursing action should the nurse expect to implement following the bronchoscopy? Keep client NPO until the gag reflex returns. What information in Mr. Stringfellow's history places him at risk for lung cancer?
This finding could indicate a pleural effusion or damage of the lung from cancer or pneumonia. The crackles present at the left apex on lung auscultation arouse concern about further...
Objective: To explore the effects of high quality nursing in patients with lung cancer undergoing chemotherapy and related influence on self-care ability and pulmonary function. Methods: 108 patients with lung cancer were grouped as the control ...